 |
MGH Community News |
 |
MGH Community News |
| May 2019 | Volume 23 • Issue 5 |
Highlights
Sections Social Service staff may direct resource questions to the Community Resource Center, Elena Chace, 617-726-8182. Questions, comments about the newsletter? Contact Ellen Forman, 617-726-5807. |
MassHealth PT-1 Portal Changes and Practice Implications
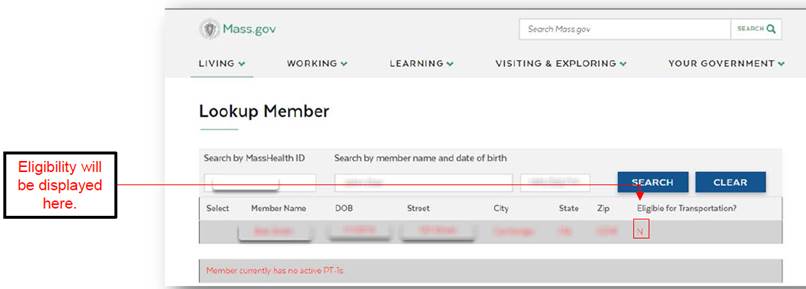
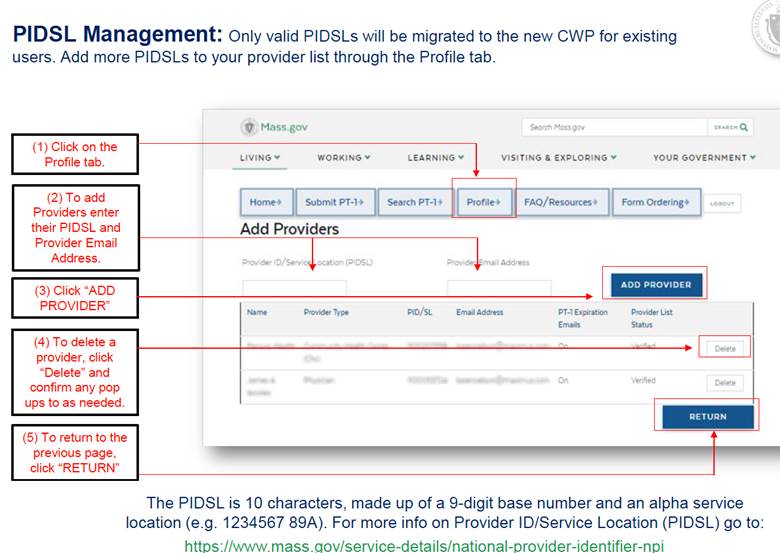
As reported last month (MassHealth PT-1 Portal Changes, April 2019), the MassHealth non-emergency transportation (PT-1) online portal (the “Consumer Web Portal or CWP”), was scheduled for an upgrade to be rolled out on May 31, 2019. Due to technical difficulties this upgrade has been delayed- we don’t have any further information at this time about a rescheduled date. Background and Reminders The PT-1 is formally called the MassHealth Provider Request for Transportation. You may recall that as of September 1, 2018, the paper form has been discontinued; since that date applications are only accepted through the CWP. Only certain disciplines may be PT-1 Authorized providers: physicians, physician assistants, nurse midwives, nurse practitioners, psychologists, dentists or dental third-party administrators, and managed-care representatives. Authorized providers may delegate others to submit on their behalf, under their auspices. PT-1 Eligibility
Key Changes Here are some of the key changes to expect from the updated CWP.
|
For More Information Want training? There are two more webinars scheduled.
To Enroll in a Webinar Please register at the MassHealth Learning Management System (LMS) via www.masshealthtraining.com Note: A MassHealth Provider ID/Service Location (PIDSL) is required for registration (MGH Social Service staff can contact Ellen Forman for our PIDSL). For questions, please contact the MassHealth Customer Service Center by email at providersupport@mahealth.net or by phone at 1-(800) 841-2900. More information on the Customer Web Portal (CWP) is available on the CWP homepage at: https://masshealth.ehs.state.ma.us/cwp/login.aspx See an updated Q&A: https://www.mass.gov/info-details/pt-1-frequently-asked-questions-faq
To Stem Displacement, Boston Will Set Value of Housing Vouchers by ZIP Code A seemingly small change in the Boston Housing Authority’s program for subsidized housing vouchers could help tenants keep up with rising rents. Boston will be the first housing authority in the country to voluntarily join the Small Area Fair Market Rents system, which allows the authority to strategically set rents for housing vouchers by ZIP code. Currently, the housing authority uses the same flat rate ($1,563 for a one bedroom) for roughly 13,000 vouchers, known as Section 8, across what is called Metropolitan Boston, regardless of the market rate of that particular neighborhood. That meant the vouchers had limited value in higher-cost neighborhoods like Beacon Hill and the Seaport. Meanwhile, residents with vouchers have historically been concentrated to lower-rent neighborhoods such as Mattapan, Roxbury, and Dorchester. “We want [residents] to live where they want to live, but we’re also hoping they live throughout Boston,” said the city’s housing chief, Sheila Dillon, “and that we see income-integrated neighborhoods. And we want to see rents in all our neighborhoods stabilized.”
The new system means the voucher rates have jumped in certain neighborhoods — for instance, a one bedroom would be $2,630 in Charlestown, an increase of $1,067. The new rate is $2,700 in the West End, a difference of $1,137. The change could go into effect July 1, following a 45-day public comment period. Bill McGonagle, the head of the Boston Housing Authority, said the system will help prevent displacement while carrying out the original intent of the federal subsidized housing program: To provide affordable housing for disadvantaged residents and desegregate them from historically deprived communities. The housing authority successfully petitioned the federal government to raise the standard rate for Greater Boston by roughly 22 percent, bringing the rate closer to market in many city neighborhoods. But that also meant that the new standard rate was higher than it needed to be in some neighborhoods, such as Mattapan and Roxbury, and officials feared that would inflate the market for those neighborhoods, affecting other residents.
The new system, McGonagle said, allows the Boston Housing Authority to strategically set the fair market rate by ZIP code, increasing — and also decreasing — the standard rate when appropriate. The housing authority oversees roughly 13,000 vouchers, and expects to receive funding for an additional 1,000 by next year, though thousands of residents remain on a waiting list. Under certain conditions, a qualifying resident who receives a Boston Housing Authority voucher can live anywhere in the Greater Boston market — and can return to the city, as well, with the new market value of the voucher. Mike Kane, director of the Mass Alliance of HUD Tenants, who advocates for affordable housing and to organize tenants, praised the new system, saying it can help residents stay in their homes or relocate to preferable neighborhoods where they may work or attend school. “It’s a pretty revolutionary idea for Boston,” he said. “Even if you had a Section 8 voucher over the last couple of years, it was really difficult to find a place in the city. This will change that.” -See the full Boston Globe article.
Update to DTA SNAP Policy for Persons with Disabilities Who Can't Make/Buy Their Own Food There are special SNAP rules for persons with disabilities getting their own SNAP benefits. DTA recently updated their guidance to clarify the policy. Although most individuals who “purchase and prepare” their food together must be in the same SNAP household, that is NOT true for individual with disabilities – of any age – who are unable to buy and cook their own food. They can still qualify for separate SNAP status as long as their own resources are being used by the helping third party to buy and prepare their food. And they do not need to be age 65 or older to qualify under this policy. For example: Tom is a 35-year-old disabled adult. He shares an apartment with a roommate, Joe. Because Tom is unable to buy and cook his own food due to his disability, Tom gives Joe money each month to buy his food and Joe prepares it. Since the majority of the meals Tom eats are purchased with his own money and are prepared separately, Tom qualifies as his own SNAP household. For more information, see DTA's guidance, and the SNAP Advocacy Guide Q&A #37. -From FoodSNAPCoalition listserv on behalf of Pat Baker, MLRI, Friday, May 03, 2019.
MBTA Piloting Visual Interpreter Services In partnership with Aira, the MBTA recently launched a six month pilot of the Access AI Pilot Program to provide indoor and outdoor wayfinding to help blind and individuals with low-vision find and use transit stations. Riders who download the Aira app can receive free access to visual interpreter services throughout the MBTA bus, subway, commuter rail, and ferry systems. The app connects users remotely to professional agents who, through the technology, are able to see the user's surroundings and offer verbal directions to help the rider get where they need to go. Check out this video to see a demonstration. During the pilot, Aira is free for anyone using it on the T. The pilot started on May 1 and will run through the end of October. Interested riders can download the app, attend a training session, or participate in a focus group. -From MassMobility - Issue 80, May 2019, EOHHS HST Office. For more information see the Boston Globe coverage.
State Officials Give Employers More Time on Paid-Leave Decision The Baker administration said this month it would give businesses nearly three more months to obtain a private-sector alternative to the state’s new paid family and medical leave program, if the businesses want to go that route. Under the 2018 law establishing the program, businesses are allowed to apply for an exemption from the state program if they can show they have a policy with benefits that are at least as generous. One big problem: Insurance companies are not yet offering any products that Massachusetts employers can buy that would exempt them from participating in the state-run program, according to AIM. AIM said that insurers are waiting until the regulations related to the program are finalized, which could be as late as July 1. But under the initial timeline, before the delay announced on Wednesday, employers would only have had until June 30 to file for an exemption from the state-run program. Now, businesses will have until Sept. 20 to file for such an exemption. But if the state rejects an employer’s exemption application, that business will be responsible for paying their contributions into the state-run program, retroactive to July 1. The agency recommended that businesses consult with their tax advisers if they plan to file for an exemption. The administration also said Wednesday that employers now have until June 30 to notify workers about their participation in the state-run program, rather than May 31. The program, part of last year’s “grand bargain” law, will cover workers for up to 12 weeks of family leave and 20 weeks of medical leave each year. While businesses and their employees must begin paying into the program July 1, employees cannot start using the paid time off until 2021. -See the full Boston Business Journal article.
Mass. General to Acquire Exeter, N.H., Hospital Massachusetts General Hospital officials said this month that they have finalized plans to acquire a community health system in Exeter, N.H., in the latest move by the Boston hospital and its parent company, Partners HealthCare, to expand beyond Massachusetts. Mass. General, along with Exeter Hospital’s parent company and Wentworth-Douglass Hospital in Dover, N.H. — which Mass. General already owns — said they plan to create a new regional health care system. State and federal regulators must approve the deal before it can be completed, a process that is expected to take about a year. Officials from the three hospitals said the transaction — which they first discussed publicly in 2018 — would strengthen health care services in New Hampshire’s Seacoast region. “We’re going to operate as a regional delivery organization in New Hampshire,” said Tony James, senior vice president of network development and integration at Mass. General. James said the merger would allow the New Hampshire hospitals to expand services in newborn medicine, cardiology, cancer care, orthopedics, and other specialty areas. “They came to us first,” James said of Exeter Hospital. “We weren’t looking to bring anyone else on board. But as soon as they presented the proposal to us, we said, ‘This makes tremendous sense for the people of the Seacoast.’” -See the full Boston Globe article.
Beware Medicare Genetic Testing Scam A scam offering free cheek swabs for DNA or genetic testing to Medicare beneficiaries is on the rise. The scammers target senior centers, care facilities, as well as set up in public places like grocery stores and ask beneficiaries to provide their Medicare number and other identifying information before providing them with genetic testing kits. In some instances, the scammer submits a fraudulent claim to Medicare for reimbursement. Medicare covers genetic testing only when a beneficiary has an order from their doctor and when the test is medically necessary. In other instances, the scammers are using the test to obtain beneficiaries’ personal information for improper uses. Advocates should caution their clients to never provide identifying information, including their Social Security number, Medicare number, or other personal information to unknown parties. Nor should beneficiaries agree to medical testing that their doctor has not ordered. To report fraud, contact 1-800-MEDICARE or the Senior Medicare Patrol at 877-808-2468. For more information, see this AARP alert. -From Justice in Aging, May 08, 2019.
MGH Connect to Wellness (Reminder) Connect to Wellness is a partnership between Massachusetts General Hospital and Boston Senior Home Care that offers on-site health and social services to residents living in three apartment buildings surrounding the hospital campus – Beacon House, Blackstone Apartments, and Amy Lowell Apartments. The aim of this community collaborative is to assist all residents in maintaining independence as they age in place by identifying social and health related needs and providing intervention. The program staff include a registered nurse, licensed independent clinical social worker, and community resource specialist who spend one day per week in each building. The schedule is as follows: Tuesday – Beacon House, Wednesday – Amy Lowell, and Thursday – Blackstone. Nursing and Community Resource Specialist office hours are held 9am-1pm while Social Work hours are 10am-2pm. Team Member Roles
Licensed Independent Clinical Social Worker
Community Resource Specialist
Team Contacts
See the flyer A Connect to Wellness webpage is coming soon as part of Community Health Improvement’s website redesign. -Thanks to Melissa Alao for sending this reminder and Molly Vespa for her assistance with this article.
Veterans Benefits Reminder- VA, the Chapter 115 Program and More Our General Resource Specialist recently attended an overview of veteran’s benefits, here’s a summary with additional material added. US Department of Veterans Affairs (VA) www.va.gov Eligibility: must have veteran status and qualifying discharge.
All veterans are encouraged to apply for benefits, even if they appear ineligible. There are two main divisions in the VA- the Veterans Benefit Administration and the Veterans Health Administration. Massachusetts also offers some state-specific benefits. Veterans Benefits Administration
Veterans Health Administration The VA Health Administration includes VA hospitals, Community-Based Outpatient Clinics, and Vet Centers. Not every veteran is automatically eligible for VA healthcare. Eligibility- must meet minimum service requirements:
However, these service requirements may not be so strict for veterans who were discharged:
Eligibility is complicated and there are numerous exceptions so all veterans are encouraged to apply. To enroll, apply in person at your local VA Health Center, online at va.gov, call 1-877-222-VETS (8387), or download VA Form 10-10EZ and mail to your local VA Medical Center. Costs of care vary depending on veteran's category and the type of care in question. Services provided for veterans can include:
You can receive VA hospital and outpatient care for any ailment, service connected or not if you are enrolled in the VA healthcare system, but you may have to pay a copayment. Advocates encourage that eligible veterans apply for Medicaid to cover care at non-VA facilities. A new policy, set to begin in June 2019, will allow veterans who can prove they must drive for at least 30 minutes to a VA facility to seek primary care and mental health services outside the department’s system. In other circumstances, VA can pay for non-VA care, but you must fill out a Claim for Payment of Cost of Unauthorized Medical Services- VA Form 10-583 and these claims are rarely successful. Massachusetts Department of Veteran's Services Find a local Veteran's Services Officer (VSO). Every town or district in MA has a VSO. VSOs primarily help access state veteran's benefits (see below), but they should also help you apply and appeal for VA compensation and pension and connect you with other services. The Chapter 115 Program- just for MA residents. MA is the only state with such a program.
MA Veterans' Bonuses - www.mass.gov/veterans-bonus-division
Location Devices for Patients Who Wander Disorientation often leads to wandering, a common and serious concern for many caregivers who worry their loved one may become frightened, lost or apt to walk into a dangerous situation. Location devices can be an option to consider as a part of a multifaceted safety plan, specific to a person’s unique needs. Using GPS tracking, these devices allow patients to be found quickly. There are a multitude of options for patients and their caregivers. Here are two websites that list GPS and related options: Details including features and pricing vary, see individual sites.
Barrier Free Playgrounds Finally the weather is starting to warm up and it's time for outdoor activities. Here is a short list of barrier free playgrounds in Massachusetts. Acton
Barnstable
Boston
Franklin
Longmeadow
New Bedford
Peabody
Pittsfield
Worcester
For a complete list of barrier free playgrounds see Index’s Recreation - Barrier Free Playgrounds Fact Sheet. -A News-brief from INDEX. Brought to you by: DisabilityInfo.org. INDEX is a program of the Eunice Kennedy Shriver Center at the University of Massachusetts Medical School.Email info@disablityinfo.org. Or, call 1-800-642-0249 or 774-455-4056.
Medicare Reminder – Appeal Rights An appeal is a formal request for review of a decision made by an Original Medicare, Medicare Advantage, or Part D plan. If you were denied coverage for a health service or item, you may appeal the decision. Before you start your appeal, make sure you fully read all the letters and notices sent by Medicare and/or your plan. Call 1-800-MEDICARE or your private health or drug plan to learn why your coverage is being denied, if the information was not provided. Your appeal letter should address the reason(s) for denial stated by Medicare or your plan. You can strengthen your appeal by including a letter from your doctor in support of your appeal. There is more than one level of appeal, and you have the right to continue appealing if you are not successful at the first level. Be aware that at each level there is a separate timeframe for when you must file the appeal and when you will receive a decision. Make sure to file each appeal in a timely manner. If there is a reason you cannot submit your appeal within the timeframe, see whether you are eligible for a good cause extension. Otherwise, your appeal may not be considered. Keep in mind that an appeal is different from a grievance. A grievance is a formal complaint that you file with your plan. Use the links below to learn more about different kinds of appeal.
If you have additional questions about the appeal process, there are resources to help you understand your rights. -From Medicare Watch, Medicare Rights Center, May 16, 2019.
Changes to Medicare Prior Authorization for DME Coming Soon In late April, the Centers for Medicare & Medicaid Services (CMS) expanded the list of durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) that require pre-authorization as a condition of payment. New codes will be added, including seven new power mobility devices (PMDs) and five new pressure surfaces including, for example, powered pressure-reducing mattresses. These changes will be implemented in phases- phase I changes will be effective either on July 22, 2019 nationally or effective on that date but only in California, Indiana, New Jersey, and North Carolina. Phase II- those only effective in certain states become effective nationwide on October 21, 2019. The new codes are detailed in this CMS announcement and the full list of all 45 prior authorization codes are available here. -Adapted from Justice in Aging, May 08, 2019.
MassHealth Disability Determination - Training PowerPoint Available Want to better understand the MassHealth disability determination process or MassHealth decision timelines? Questions about the CommonHealth coverage type (including the deductible when applicable)? Check out the PowerPoint for the recent MassHealth training MassHealth and Disability. Some excerpts:
See the full MassHealth and Disability Powerpoint.
Families USA is excited to announce the launch of Consumers First: The Alliance to Make the Health Care System Work for Everyone! Consumers First is a new alliance that brings together powerful interests from consumers, children, employers, labor unions, and primary care providers working to change the fundamental economic incentives and design of the health care system. Our work is to realign the incentives and design of health care so that the system truly delivers the health and high quality health care that all families across our nation deserve. For too long, there has not been a sophisticated, non-partisan group at the table focused on the economics and fundamental design of the health care sector. Instead, policymakers turn to members of the health care industry -- often hospitals, doctors, pharmaceutical companies, and insurance plans -- to serve as proxy for their patients and enrollees. Consumers First will counterbalance those interests and find key opportunities to change federal and state laws and policy to redirect the economic incentives and design of the health care sector. The first product from Consumers First is Our Call to Action. It includes six policy domains representing the underlying distortions within the health care system that need immediate action, and will be the focus of Consumers First's work in 2019 and beyond. Consumers First will also be releasing a targeted agenda for Congress and the Federal Administration that will crosscut the six policy domains, build a broad coalition, and conduct key nonpartisan stakeholder dialogue with federal agency leadership and congressional champions. Ultimately, our aim is to reshape the way in which our nation conceives of health and pays for health care. This includes, for example, addressing flaws in our fee-for-service system that reward volume and specialty care over primary and behavioral health care, changing the ways that we develop and empower the U.S. health care workforce, or how we address health care data blocking, hospital consolidation, and a host of other fundamental distortions in the health care sector The Consumers First steering committee includes a set of key, non-partisan, national groups including: First Focus, Pacific Business Group on Health, American Benefits Council, American Academy of Family Physicians, American Federation of State, County, and Municipal Employees, American Federation of Teachers, and Families USA To sign up for updates about Consumers First, please email your name and organization to ConsumersFirst@familiesusa.org. -From New Initiative: Consumers First Alliance, Patrick Willard, Families USA, May 14, 2019.
Rental Arrearage Assistance Program Budget Proposal Senator Pat Jehlen of Somerville has proposed a budget amendment (Amendment #7970) to establish and fund a new pilot program- the Rent Arrearage Assistance Program (RAAP) under the Residential Assistance for Families in Transition (RAFT) program. The program would provide cash assistance for up to four months of back rent or mortgage payments for families, individuals, and unaccompanied youth with incomes up to 50% of Area Median Income (AMI). At least 50% of funding for the program would need to be provided to households with incomes at or below 30% AMI. Cash assistance would be payable directly to the landlord or mortgage lender, and applicants would NOT need to be in eviction or foreclosure proceedings in order to be eligible for assistance. Otherwise eligible households would qualify for this resource once they can document that they are in arrears on rent or mortgage liabilities. The amendment also would add $7 million to the RAFT line item for the purposes of administering the pilot rent arrearage assistance program, increasing the line item total from $20 million to $27 million Why does this matter? The intersection of soaring housing costs, an inadequate supply of affordable homes, and stagnant wages for workers often leads to the experience of housing instability, which is felt most deeply in households with the fewest resources. Among individuals and families with the lowest incomes across the Commonwealth, housing costs routinely consume an outsize portion of household income. Many pay far more in monthly housing costs than the 30% of household income that is typically considered to be affordable, meaning that they experience a cost burden. In fact, according to The Gap: A Shortage of Affordable Homes 2018, published by the National Low Income Housing Coalition (NLIHC), 60% of Massachusetts renters earning less than 30% AMI are severely cost burdened, paying more than half their income on rent. This compares with just 2% of middle-income households earning between 81% and 100% of AMI. Further, The Gap reports that the Commonwealth has only 46 rental homes affordable and available for every 100 of the state’s households earning less than 30% AMI, compared with 99 homes for each of the state’s 100 middle income households. This leads to those individuals and families with the fewest resources being disproportionately likely to live in housing that they cannot truly afford, straining their already limited budgets. For the state’s low and moderate-wage earners, simply working full-time does not provide sufficient income to remain stably housed. According to NLIHC’s Out of Reach: The High Cost of Housing 2018, a single-income Massachusetts household would need to earn $28.64 per hour in order to afford rent on a modest two-bedroom home. This is equivalent to working 95 hours per week at the state’s recently increased $12 per hour minimum wage, making Massachusetts one of the costliest states in the nation for housing. For people experiencing housing instability and limited financial resources, a single emergency can drive the household into a downward spiral of missed rent or mortgage payments, eviction, and homelessness. Most eviction cases begin when a renter cannot pay the rent. When households fall on hard times and have no way of avoiding an eviction due simply to being unable to pay their rent, the ensuing experiences can unleash a wave of consequences and trauma felt for years to come. The best solution to the problems that arise from an eviction is to prevent that eviction from ever taking place at all. For households at risk of eviction and homelessness due to nonpayment of rent, the clearest and most effective solution is an immediate infusion of cash assistance to help pay down their arrears and keep them in their home. Rental arrearage assistance is a policy solution already proven to work in the Commonwealth. A 2003 DTA analysis of its previously administered rent arrearage assistance program indicated that 96% of recipients maintained stable housing and did not require deeper assistance in the form of an emergency shelter stay during the following 12 months. Further, 75% of families attained self-sufficiency, and did not need additional arrearage payment assistance during the following calendar year. See the RAAP Senate amendment fact sheet Want to support the amendment? See the call script and talking points. - From Kelly Turley, MA Coalition for the Homeless, May 14, 2019.
Fact Sheet- Medicaid Non-Emergency Medical Transportation: A Critical Benefit at Risk As reported last month (April 2019), the Trump administration is proposing making non-emergency medical transportation (PT-1) an optional benefit- making it available at a state’s option. Justice in Aging has created a fact sheet, excerpted below. What is NEMT and why is it important? Non-emergency medical transportation (NEMT) is currently a required Medicaid benefit that provides transportation to and from non-emergency health care appointments and services. Currently, NEMT serves over 7 million Medicaid enrollees across the U.S. Many of these enrollees are older adults who use NEMT to access services such as dialysis, substance use disorder/behavioral health care, adult day health care, preventive care, specialist visits, and physical therapy/rehabilitation.3 Indeed, NEMT is a lifeline for those, who, due to cognitive and physical changes, may have a reduced ability to drive or use public transportation. It is critical for low-income patients who do not have resources to pay for transportation services out-of-pocket. A robust NEMT benefit also helps address health equity issues. For example, nearly 40% of women older than 75 do not drive, increasing the risk of isolation and gaps in care.Additionally, in Iowa, for example, Black and Hispanic Medicaid enrollees were respectively 83% and 31% more likely than non-Black and non-Hispanic enrollees to have unmet care needs due to lack of transportation. NEMT also helps individuals residing in rural areas and individuals who have recently sustained injuries or are recovering from surgery. Medicaid NEMT has proven to be a cost-effective benefit. Assisting individuals in getting to their routine medical appointments enables them to receive preventive care and adhere to treatment regimens that in turn avoid medical emergencies, hospitalizations, and institutionalization. For older adults who need long-term services and supports, consistent and reliable transportation to and from medical appointments can be the difference between aging in the community and moving into an institution. Medicaid spends less than 1% of its total budget on NEMT, but yields a significant return on investment. Recent data has shown that NEMT has resulted in a specific return on investment for both wound care for diabetics and dialysis.7 One Florida study estimated that NEMT trips help to prevent one-day stays in hospitals, resulting in savings of $11 for every $1 spent on transportation. What is the threat to NEMT? The Centers for Medicare and Medicaid Services (CMS) has signaled that it will propose a regulation to make the mandatory NEMT benefit optional for states. States could then choose to amend their Medicaid rules to eliminate the benefit. When states face difficult choices balancing budgets, optional benefits are often the first that are eliminated or reduced. Since transportation is a critical component to accessing health care for low-income older adults, changing the benefit from mandatory to optional would likely have negative—and expensive—consequences for the health of those enrolled in Medicaid. -See the full Justice in Aging fact sheet, including advocacy opportunities and resources for more information.
Assisted-Living Closures a Troublesome Trend Cape Cod legislators say they are concerned and surprised about recently announced plans to shutter two assisted-living facilities on the Lower Cape. This month the owner of Wingate Residences at Brewster Place notified residents and staff it plans to close the assisted-living facility on or about Aug. 2. Four miles down the road, the owner of The Royal at Harwich Village notified residents April 26 that it intends to close that facility by July 26, according to officials from the state Executive Office of Elder Affairs. “It’s a troublesome trend,” state Sen. Julian Cyr, D-Truro, said Thursday. “We don’t know yet if (the closings) are related.” The summer shutterings also come as a surprise because assisted-living facilities rely on private pay instead of government reimbursement and, at least in theory, have a more flexible business model, Cyr said. Officials from the Royal Health Group, which also owns four nursing homes on Cape Cod — The Royal Cape Cod Nursing Center in Buzzards Bay, Royal Cotuit, Royal Nursing Center in Falmouth and Royal Megansett Nursing & Retirement Home in North Falmouth — did not respond to calls and emails asking for comment. Wingate Healthcare chief operating officer Jill Bosa said in a statement that the company had exhausted “all other options” before coming to what she called the difficult decision to close Wingate Residences at Brewster Place.
Bosa declined in an email Thursday to elaborate or answer other questions about the plans of Wingate Healthcare. The organization owns 35 senior living facilities in three states, and celebrated the opening of a new assisted-living facility in Haverhill this past fall. Since 1995 only 16 assisted-living residences have closed, not including the two recently announced closings, state officials said. On the Cape, the trend also has been toward growth, with the Mill Hill Residences in West Yarmouth opening during the summer of 2017 and the Decatur House Assisted Living Residence in Sandwich recently receiving approval to expand. When assisted-living centers do close, they must notify residents and state officials 90 days in advance, according to the state Executive Office of Elder Affairs. “My husband and I toured a facility today,” said Susan Ostrander, of South Dennis. “We’re trying to find places that are in her (aunt’s) price range and are (for) the middle class.” But buy-ins at some places range from $25,000 to $250,000, Ostrander said. “There is no affordable housing option for these people,” she said. The family thought Wingate Residences at Brewster Place, with its monthly rent of $4,000 and move-in fee of $2,250, was the perfect solution for their widowed aunt, Ostrander said. “The meals are delicious” and the grounds beautifully maintained, she said. “You never had a hint there might be a financial issue with this facility.” William Bogdanovich, owner of Liberty Commons nursing home and the Victorian assisted-living residence in Chatham, said he did not know why the two assisted-living centers were closing, but he said finding workers is a common challenge for people in the senior care industry. “It’s harder than it’s ever been” in his three decades of working in the industry, Bogdanovich said. People also may call the office’s assisted-living ombudsman for help at 617-727-7750 and look up assisted-living residences at mass.gov/assisted-living. -See the full Cape Cod Times article.
Bill Would Make it a Felony to Assault Health Providers Elizabeth Dalton was working as a cardiac intensive care nurse at Brigham and Women’s Hospital on April 10, 2015, when a patient’s father brandished a hunting knife. Dalton said the man was threatening, irrational, and frightening. “I thought my life was in danger,” she said. When the patient’s roommate yelled at the man to put the knife down, Dalton ran past him and escaped. The man was allowed back into the hospital eight hours later with a reprimand. “It’s time we stopped treating assaults on health care providers as just part of the job,” Dalton told members of the Legislature’s Judiciary Committee at a public hearing this month. A bill sponsored by Rep. Paul Tucker, D-Salem, and Sen. Michael Brady, D-Brockton, S.838/H.1578, would change assaults on health providers, emergency medical technicians or ambulance attendants from a misdemeanor to a felony offense, punishable by up to five years in prison. Tucker said the legislation “will set a tone that the assaults on these workers who are trying to do their job will not be tolerated.” The Massachusetts Nurses Association is pushing for the bill. The union is also pushing for a separate bill that would require health care employers to develop and implement programs to reduce workplace violence. According to the U.S. Occupational Safety and Health Administration, from 2002 to 2013, healthcare workers were four times more likely to experience serious workplace violence than the average private sector worker. Most injuries were caused by patients. A 2014 survey of more than 3,700 nurses by the American Nurses Association, cited by OSHA, found that 21% of registered nurses and nursing students reported being physically assaulted in a 12-month period. A 2009-2011 survey of more than 7,100 emergency room nurses by their trade association found that 12% of emergency department nurses experienced physical violence during a seven-day period. Erin Johnson, a nurse at Providence Behavioral Health Hospital who is involved with the Massachusetts Nurses Association, said health care workers account for nearly 70% of all non-fatal workplace assaults. She said more than 80% of emergency department nurses have been the victim of workplace violence. A Massachusetts survey found nearly three-quarters of nurses reported that violence was a serious or somewhat serious problem in their workplace. -See the full Mass Live article.
Baker Administration Pledges Major Reforms for Troubled Foster Care System The Baker administration this month announced major changes to the state’s troubled foster care system that it says will improve the lives of thousands of children, ease caseloads for their swamped social workers, and more aggressively recruit and retain foster families. The plan, presented as a joint agreement between the state’s Department of Children and Families and SEIU Local 509, the union that represents foster care workers, promises to boost the number of social workers who communicate directly with foster families. DCF will also hire 11 additional employees to recruit more foster families, and offer more training for foster families who are struggling to care for severely traumatized children. And the Baker administration is promising to initiate listening sessions statewide to better understand the roadblocks families face in obtaining mental health care for foster kids. The plan will not require changes in law. The administration did not say how much it would cost or how it would be funded, but Governor Charlie Baker left the door open for additional spending.
“We’ve added roughly $150 million to the DCF budget over the course of the past four years,” he told reporters Tuesday. “It’s a place where we continue to make investments. If it turns out we need to make additional ones, we will.” “The Baker administration says they are committed to fixing this system, and we will take them at their word,” said Peter MacKinnon. “If attention gets shifted, we will call people out on that.” Marylou Sudders, the state’s health and human services secretary, said in a phone interview that the changes include a top-to-bottom review of policies, in the hope that doing so will draw more prospective foster parents. For instance, she said, decade-old rules that require foster children to have at least 50 square feet in a home don’t make sense when the department is trying to encourage more relatives to step forward and take in children. Some relatives’ houses just miss that mark. Current regulations also eliminate as candidates for fostering any relatives who have had minor scrapes with the law when they were much younger — offenses that do not affect their ability or the safety of raising children today. “I see these as common-sense reforms,” Sudders said. Child advocates said they welcomed the promised changes. Mary McGeown, president of the Massachusetts Society for the Prevention of Cruelty to Children, agreed. She said surveys of foster families conducted by her organization for DCF found that families are clamoring for better communication with the department. McGeown said her organization is also discussing with DCF ways to improve respite care for foster families by training volunteers who would provide a few hours’ or a couple days’ care, allowing parents a much needed break. In its announcement, the Baker administration said it would also provide emergency day care for 10 of the busiest DCF offices, and it plans to offer day care for all its offices in the next year. Many of these offices have been operating as de facto child care centers, with even small children playing in the offices all day as social workers search for foster homes to take them in. The administration also laid out a timetable for major technology upgrades at DCF, detailed recently in the Globe, to improve communication with thousands of foster parents and to overhaul the process for placing abused and neglected children who are removed from their homes at night. A new, secure intranet system was slated to go live on earlier this month, allowing foster families to communicate directly with DCF. And a new after-hours hot line database will track open foster homes in real time. Sudders said that database will be operational by Nov. 1. The lack of such capabilities in a state known as a technological hub has sparked withering criticism of the agency. Recent Globe stories featured social workers who drove through the night with children, as the department’s supervisors, hampered by a lack of a real-time database, searched for available foster homes. -See the full Boston Globe article.
Immigrant Families in Public Housing Units Threatened by Trump Administration Proposal The Trump administration is proposing a rule could bar whole families from public housing and certain other types of federally subsidized housing programs, including Section 8, if any household member is an undocumented immigrant. Now, tenants can live in federally supported housing as long as at least one household member is documented. Ben Carson, head of the U.S. Department of Housing and Urban Development, said the change would ensure that “our scarce public resources help those who are legally entitled to it.” He cited long waiting lists for subsidized housing. Current regulations prohibit undocumented residents from obtaining public housing and certain other federal housing subsidies, and they require tenants under 62 to submit proof of their status. But undocumented immigrants can opt out of submitting evidence and thus “declare” that they are not eligible. The regulations allow them to live in subsidized apartments as long as one family member is documented, but ineligible tenants get no subsidy, so the family’s rent is higher. The proposal would require all tenants under 62 to provide evidence, and family members’ citizenship or eligibility status would be checked in a federal database. Undocumented residents could not head the household or sign a lease, ruling out families where only a child is a citizen. “Mixed” status families could get extensions to stay, but only up to 18 months. Johnston said the housing authority intends to send a letter this week to families that could be affected, “informing them that there is a proposed change but emphasizing that it is not yet in effect” and that officials “hope that it is never implemented.” “We don’t want these families to move out because of fear,” he said. A 60-day public comment period ends June 30. There’s no citizenship requirement to live in state-funded subsidized housing. The city housing authority has switched most of its state low-income housing to federal to take advantage of federal funding programs. -See the full Cambridge Day article.
HHS Issues Proposal to Gut Health Care Rights Rule This month, the U.S. Department of Health & Human Services (HHS) Office for Civil Rights issued a notice of proposed rulemaking to rewrite the regulations implementing the Health Care Rights Law, Section 1557 of the Affordable Care Act. The law prohibits discrimination in healthcare on the basis of race, color, national origin, sex, age, and disability in federal health programs and activities. The proposed rule attempts to limit means for victims of discrimination to seek redress and guts affirmative protections, including for LGBTQ people and people with limited English proficiency. To learn more about the current Health Care Rights Law, read the Justice in Aging issue brief. - From Justice in Aging, May 24, 2019.
New Trump Rule Protects Health Care Workers Who Refuse Care for Religious Reasons The Trump administration issued a new rule this month that gives health care workers leeway to refuse to provide services like abortion, sterilization or assisted suicide, if they cite a religious or conscientious objection. The rule, issued by the Department of Health and Human Services, is designed to protect the religious rights of health care providers and religious institutions. According to a statement issued by HHS's Office for Civil Rights, the new rule affirms existing conscience protections established by Congress. Last year OCR Director Roger Severino made it clear that defending religious freedom was his primary goal when he created a new Division of Conscience and Religious Freedom. "Never forget that religious freedom is a primary freedom, that it is a civil right that deserves enforcement and respect," Severino said when he created the division.
As part of that change in focus, HHS in the last week also changed the Office for Civil Rights' mission statement to highlight its focus on protecting religious freedom. "This rule allows anyone from a doctor to a receptionist to entities like hospitals and pharmacies to deny a patient critical — and sometimes lifesaving — care," said Fatima Goss Graves, president and CEO of the National Women's Law Center, in a statement. -See the full NPR story.
Proposed HUD Rule Would Strip Transgender Protections at Homeless Shelters The Department of Housing and Urban Development this month proposed a new rule that would weaken Obama-era protections for homeless transgender people, allowing federally funded shelters to deny people admission on religious grounds or force transgender women to share bathrooms and sleeping quarters with men. The proposal is the latest move by the Trump administration to weaken protections for transgender Americans, including a Department of Defense ban on transgender troops and a Department of Health and Human Services proposal allowing medical providers to deny treatment to transgender people on religious grounds (see accompanying story). In 2017, the HUD website removed links to documents that guided emergency shelters on how best to serve transgender people facing homelessness and comply with agency regulations. It also withdrew policy proposals requiring HUD-funded emergency shelters to post notices informing people of LGTBQ rights and protections. Transgender advocates characterized it as a ‘‘heartless attack’’ and said it signifies an ‘‘escalation of the Trump administration’s broader plan to erase transgender people from federal regulations and legal interpretations.‘‘ ‘‘It completely guts the Equal Access Rule,’’ said Mara Keisling, executive director of the National Center for Transgender Equality. ‘‘The Trump administration is, once again, targeting the most vulnerable trans people by empowering shelters to turn people away and deny them equal access to services.’’ One in 3 transgender people has experienced homelessness — including 1 in 8 in the past year, putting them at risk of physical and sexual violence and being forced into sex work, according to the National Center for Transgender Equality. Seventy percent of transgender people who tried going to a shelter in the past year were kicked out for being transgender, were physically or sexually assaulted, or faced another form of mistreatment because of their gender identity, the center said. -See the full Boston Globe article.
Trump Administration Proposal Would Make it Easier to Deport Immigrants Who Use Public Benefits The Trump administration is considering reversing long-standing policy to make it easier to deport U.S. legal permanent residents who have used public benefits, part of an effort to restrict immigration by low-income people. A Department of Justice draft regulation, seen by Reuters, dramatically expands the category of people who could be subject to deportation on the grounds that they use benefits. Currently, those legal permanent residents who are declared to be a “public charge,” or primarily dependent on the government for subsistence, can be deported - but in practice, this is very rare. The draft regulation would use a more expansive definition to include some immigrants who have used an array of public benefits, including cash welfare, food stamps, housing aid, or Medicaid. While the plan is at an early stage, might not become official government policy, and is likely to attract lawsuits, it is one part of efforts by the Trump administration to restrict legal immigration, in addition to its efforts to reduce illegal immigration to the United States. The full possible impact is not known, but the change in policy could affect permanent residents - also known as “green card” holders - who are legally entitled to use public benefits soon after their arrival in the United States, such as refugees. U.S. law allows for the deportation of immigrants who have become “public charges” within five years of admission if their reason for seeking help preceded their entry to the United States - for example, if they had a chronic health condition that was not disclosed. But due to a 1948 ruling, the deportation of immigrants for using public benefits has been strictly limited to cases in which the government has demanded payment for public services, and the person has failed to pay. Immigration lawyers said they have rarely if ever heard of someone being deported for using public benefits. The draft rule indicates the government would override that precedent to allow for deportation of some permanent residents who have used certain public benefits within five years of admission. For the plan to go into effect, it would be subject to public comment, after which it could be revised. Attorney General William Barr would then have to sign off on it. The public benefits in question include Supplemental Security Income (SSI), given to disabled and older people; the Supplemental Nutritional Assistance Program (SNAP), commonly known as food stamps; Section 8 housing vouchers; many Medicaid benefits; and Temporary Assistance for Needy Families (TANF), a cash assistance program.
According to federal policy, many permanent residents do not qualify for public benefits unless they have had a green card for five years, making it unlikely they could be targeted for deportation on the basis of “public charge” even under the draft rule. And the effort to tighten the rules could affect thousands of immigrant veterans, refugees and asylees, who are eligible to receive many benefits without time restrictions. Active members of the military would not be affected. ‘New Territory’Immigrant advocates said the impact of the possible change is unclear, because it would be such a departure from long-standing practice. “We’re in new territory here because this has never been tested,” said Charles Wheeler, an attorney with the Catholic Legal Immigration Network non-profit group. “I’m concerned that it’s going to be targeted at permanent resident aliens who otherwise thought they were free and clear to receive SSI and other public benefit programs.” The Justice Department’s draft proposal is based on a similar plan by the Department of Homeland Security (DHS) to significantly broaden the definition of what it means to be a public charge. While DHS can decide whether to grant or deny immigration benefits, DOJ’s immigration judges can also decide whether a resident ought to be deported. In addition to considering new standards for deporting legal residents, the DOJ is also looking at requiring foreigners seeking permanent residency status to submit a declaration to an immigration judge that demonstrates their self-sufficiency. The form asks for a detailed listing of assets, income, and debts, among other information. -See the full Reuters article. For more information see the Public Charge & Deportation FAQ for Advocates and Community Members from Protecting Immigrant Families. Excerpt: Should I stop using public benefit programs just to be safe? We recommend that you continue to get the help you need. Using health care and other services can help you and your family become healthier, stronger and more employable. You can stay tuned for any changes that may occur, and can consult with an immigration attorney if you have questions about your individual situation. If your family plans to apply for a green card or visa inside the United States, we recommend that you continue to use health, housing, and nutrition programs like SNAP, Medicaid, or Section 8 housing assistance that help your family. If your family plans to apply for a green card or visa outside of the United States, you should talk with an expert for advice on your case before making any decisions. For free or low-cost options near you, visit www.immigrationadvocates.org/nonprofit/legaldirectory. Help is available in many languages. Related: New Handout for Previous Public Charge Proposal Protecting Immigrant Families has created a helpful and clear handout for the public that explains the previously proposed changes to Public Charge that would change the types of public benefits that could count against an immigrant in public charge considerations. (These previous changes also are not in effect at this writing, but final rules may be coming soon.) Public Charge: Getting the Help You Need (currently English only; translations expected- check their website:https://protectingimmigrantfamilies.org/community-education-resources/).
Most Generics are Manufactured Overseas and Safety Concerns are Mounting The majority of generics bought in the US are made overseas: Roughly 40 percent are manufactured in India; 80 percent of the active ingredients in all of our drugs, whether brand-name or generic, are made in India and China. As one drug-ingredient importer put it, “Without products from overseas, not a single drug could be made.” The vast amount of overseas manufacturing presents an enormous challenge for the Food and Drug Administration (FDA), which must safeguard thousands of drugs manufactured abroad by foreign companies. The FDA contends that it has a reliable review system for all approved drugs. “The FDA inspects all brand-name and generic manufacturing facilities around the world which manufacture product for the US market to confirm they meet FDA’s requirements for manufacturing process,” the agency said recently. It asserts that all the generics it approves are bioequivalent to the brand (meaning, they reach the same level of absorption in the blood). But American physicians — particularly those who prescribe drugs that require precise dosing — are questioning the FDA’s ability to police overseas manufacturing. Are all those drugs clinically equivalent? And do the generic drugs that the agency approves actually meet the FDA’s standards, since the agency’s own investigators have discovered staggering fraud in a number of overseas drug plants? Over the past two decades, US pharmaceutical companies have been moving their manufacturing to China, India, and other foreign markets to slash labor and production costs. Foreign drug manufacturers, in turn, have been seeking approvals from the FDA to gain entry to our pharmaceutical market — the world’s largest and most lucrative. By 2005, the Food and Drug Administration had more drug plants to inspect overseas than it did within US borders. While the agency has struggled to police a global drug supply, US patients have faced a perfect storm of consequences. The ever-climbing prices of brand-name drugs have led to our reliance on the lowest-cost manufacturers overseas. Recently, dozens of versions of the generic blood pressure medicines — valsartan and losartan — have been recalled, due to ingredients manufactured in China that contained a carcinogen that had gone undetected for years. Recalls due to flawed manufacturing have contributed to chronic drug shortages. The US makes almost none of its own antibiotics anymore, leaving us in a perilous state of pharmaceutical dependence on other countries, a situation that has become a national security risk. Solving these problems requires a multi-pronged solution to reduce brand-name drug prices, overhaul the FDA’s foreign inspection program and revamp a system in which regulators rely on company-submitted data to verify drug quality. But along with these efforts must come a rethink of who makes our drugs where. Shouldn’t some percentage of our essential drugs be made on US soil? Senator Elizabeth Warren, now running for president, has proposed that the US government get into the business of manufacturing generic drugs as a way to address the public health crisis of unaffordable medicine. A newly launched non-profit drug manufacturer, Civica Rx, headquartered in Utah, aims to manufacture drugs in short supply within the US, and disclose its manufacturing locations on patient dispensing labels. If these efforts gain traction, they could help to remove the question marks currently hovering over the low cost generics that doctors and patients rely on: Where were these manufactured, under what conditions, and will they really be as clinically effective as the brand-name drugs? -See the full Boston Globe article.
Competing Visions for Shattuck Campus: Behavioral Health and Homeless Services vs. Park Land
Lemuel Shattuck Hospital is set to relocate its operations from the southwestern edge of Franklin Park, but the future of the state-owned land it's on is uncertain. Both state officials and park advocates see the move as an opportunity, but have conflicting ideas about what to do with the land once the hospital is gone. Meanwhile, a state official said it is unlikely the 13-acrea Shattuck campus will be given back to the city. "We've been clear that this is a public health asset that the commonwealth holds," Executive Office of Health and Human Services Undersecretary Lauren Peters told WGBH News. The state envisions a new set of buildings across the Shattuck campus that would house both the chronically homeless and the hard-to-site services that will not move when Shattuck relocates to the Newton Pavilion in the South End in 2021. Among the services are a methadone clinic and other behavioral health services and residential treatment programs. Health and Human Services, the Department of Public Health, and the Interagency Council on Housing and Homelessness have already received the first of two required approvals to lease two acres of the Shattuck campus to a “developer/provider of Low Threshold Housing for the chronically homeless," according to a preliminary project proposal before the state's Asset Management Board in 2017. The proposal described a target size of 75 to 100 units, but some are in favor of the state's vision for even more housing and services on the Shattuck campus. "Boston can be a difficult place to find housing for anybody, let alone somebody who may have CORI issues, or doesn't really have much of an income," said Zack DeClerck, a person in long-term recovery and advocate on the Shattuck campus community advisory board. "I'd like to see more on the site, and I think it can be done without destroying the park." Others, like Karen Mauney-Brodek, president of the Emerald Necklace Conservancy, insist the state restore the entire Shattuck campus to the city, and pursue other sites for such housing and services. The next public meeting about the future of the Shattuck campus is scheduled for the end of June. -See the full WGBH article.
Social Security Trust Fund Solvency Estimates Projections Much Improved Last month the Board of Trustees released its 2019 Social Security Trustees Report. The report provides an annual assessment of the health of the Social Security program’s finances. Social Security has two trust funds — a trust for retirement and survivors’ benefits, called the Old Age and Survivors (OASI) trust, and another trust for disability insurance (DI). The report finds that the Social Security DI trust fund is now projected to be fully funded another 33 years, until the year 2052. This projection is 20 years longer than what was estimated just last year, and is a result of years of declining DI applications and disability beneficiaries.
The Trustees’ Report also finds that the retirement and survivors trust fund will be fully funded until the year 2034, after which it will be able to pay individuals approximately 77 percent of the benefits they are owed over the next 75 years. Millions of Americans depend on Social Security to meet their needs as they age, or when they are faced with serious disabilities or the untimely death of a family member. We must support and fund this vital program to ensure that we do not leave behind the people who need it most. -From Justice in Aging, May 09, 2019.
National Eating Disorders Parent Toolkit The National Eating Disorders Association (NEDA) Parent Toolkit is for anyone who wants to understand more about how to support a family member or friend affected by an eating disorder. You will find answers to your insurance questions; signs, symptoms and medical consequences; information about treatment and levels of care; and questions to ask when choosing a treatment provider. Sections include:
View or download the toolkit: https://www.nationaleatingdisorders.org/parent-toolkit -Thanks to Lindsey Krenzel for sharing this resource.
|